When interacting with someone who has experienced trauma, understanding the underlying condition is crucial for providing meaningful support. Many well-intentioned people inadvertently cause harm through misguided words or actions, often stemming from a lack of awareness about what trauma survivors actually experience. To build empathy and avoid potentially damaging responses, it’s essential to first grasp the fundamental nature of post-traumatic stress disorder and how it affects those who live with it.
If you’re supporting someone with PTSD in an ongoing role, understanding the broader responsibilities and challenges of caregiving can provide important context for avoiding these mistakes. By educating ourselves about PTSD’s symptoms and impact, we can better recognize why certain approaches may be helpful or harmful. Let’s begin by examining what PTSD truly entails and how it manifests in daily life.
Post-Traumatic Stress Disorder: A Quick Overview
Post-Traumatic Stress Disorder (PTSD) is a serious mental health condition that can develop after a person experiences or witnesses a traumatic event. This could include situations like a serious car accident, natural disasters, terrorist acts, war, domestic violence, mass shootings, the unexpected death of someone you love, or violent personal assaults.
People with PTSD may relive the trauma through distressing dreams and flashbacks and may experience feelings of isolation, irritability, and guilt. For someone with PTSD, nightmares also cause difficulty sleeping, which leads to lower energy and a loss of interest in activities they once enjoyed.
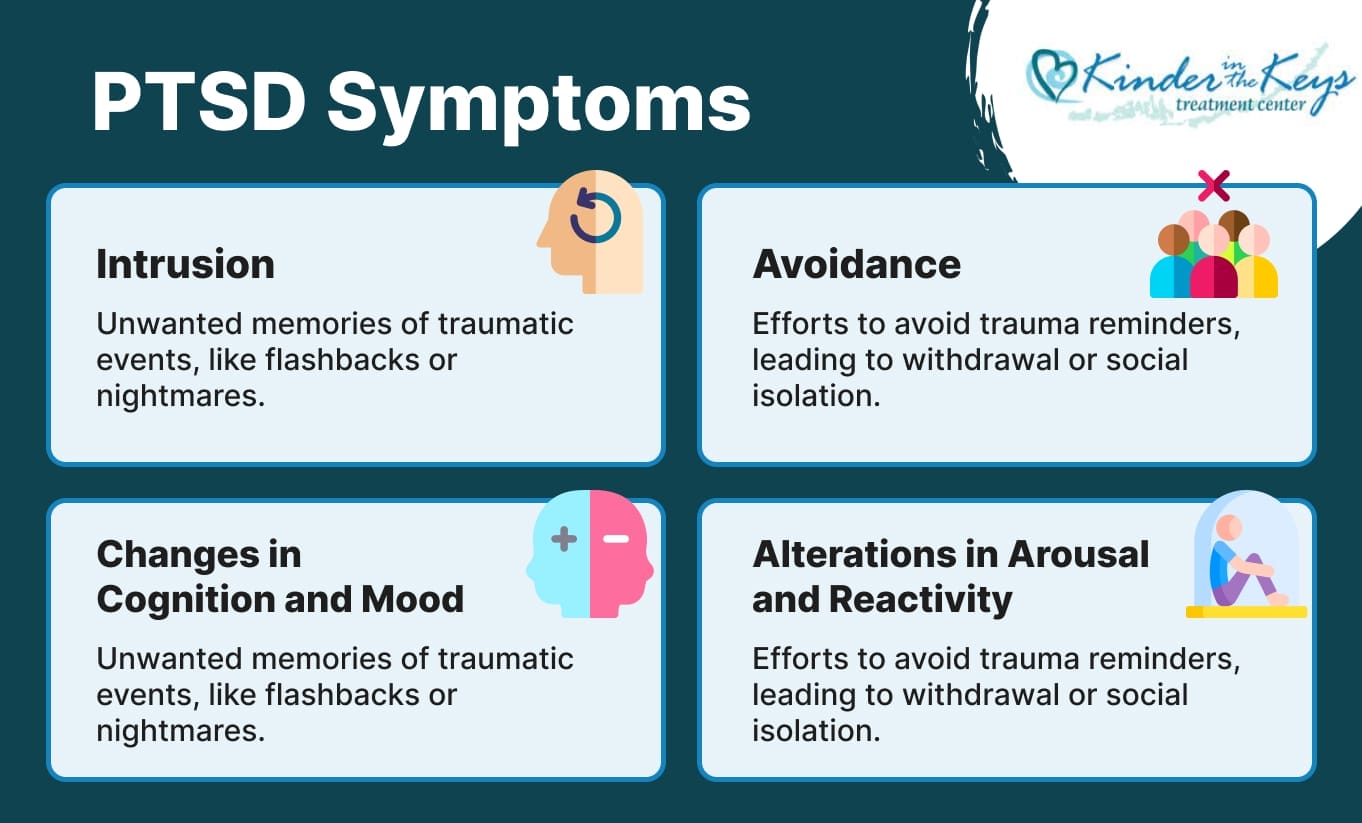
PTSD Symptoms
Understanding the symptoms of PTSD is the key to recognizing why certain actions or words can be harmful and how a traumatic incident can cause someone to develop debilitating symptoms of PTSD. For many, especially women, understanding PTSD symptoms in women can shed light on the unique ways trauma manifests and help guide more effective paths to healing. The symptoms are typically grouped into four categories:
- Intrusion: Unwanted and intrusive memories of the traumatic events, which can manifest as flashbacks or nightmares.
- Avoidance: Deliberate efforts to avoid trauma reminders, including people, places, activities, and situations that bring back memories. This can look like withdrawal or social isolation.
- Changes in Cognition and Mood: This includes feelings of detachment or estrangement from others, persistent negative emotions (such as fear, horror, anger, guilt, or shame), distorted beliefs about oneself or others (e.g., “I am bad,” or “No one can be trusted”), and diminished interest in significant activities. This is where strategies for overcoming hopelessness can be particularly effective.
- Alterations in Arousal and Reactivity: These are manifested as aggressive, reckless, or self-destructive behavior, sleep disturbances, being easily startled, difficulty concentrating, or extreme vigilance. They impact a person’s daily functioning.
Related Article: How to Recognize PTSD from Narcissistic Abuse
Worst Thing To Do To Someone with PTSD
When someone is battling post-traumatic stress disorder (PTSD), you should be careful to approach them with sensitivity and understanding. Unfortunately, some actions and words exacerbate their condition, making it even more challenging for them to cope with daily life.
Understanding the worst things to do or say to someone with PTSD can help you foster a supportive environment while avoiding inadvertently causing harm. Here are some sentences and attitudes that can actually harm a person with post-traumatic stress disorder, even if you’re trying to help.
“It’s all in your head.”
This phrase can be deeply invalidating for someone struggling with PTSD. While the brain is indeed where trauma processing occurs, dismissing someone’s experience as purely psychological minimizes the very real physiological and emotional impact of their condition. PTSD involves measurable changes in brain structure and function, affecting how memories are stored and retrieved. When we tell someone their suffering is “just in their head,” we unintentionally communicate that their pain isn’t legitimate or worthy of attention, which can increase feelings of isolation and shame.
“It’s not that bad.”
Minimizing someone’s trauma experience, even with good intentions, can be profoundly hurtful. Each person’s capacity to process and cope with traumatic events is unique, influenced by factors like previous experiences, support systems, and individual resilience. What might seem manageable to one person can be overwhelming to another. When we downplay someone’s struggle, we risk making them feel misunderstood and alone in their healing journey, potentially discouraging them from seeking the help they need.
“Just relax.”
For someone with PTSD, relaxation isn’t simply a choice or a matter of willpower. The condition involves a dysregulated nervous system that remains in a heightened state of alertness, making it genuinely difficult to achieve calm. Suggesting that someone “just relax” oversimplifies the complex neurobiological processes at work and may leave them feeling frustrated or inadequate. Instead of offering relief, this advice can increase their sense of being misunderstood and add pressure to their already challenging situation.
“How many people did you kill?” (And Other Intrusions)
Intrusive questions about traumatic details can retraumatize someone and violate their sense of safety. These inquiries, often driven by curiosity rather than genuine concern, can trigger flashbacks, nightmares, and intense emotional distress. Privacy around traumatic experiences is essential for healing, and individuals should have complete control over when, how, and with whom they share their stories. Respecting these boundaries demonstrates genuine care and creates space for trust to develop naturally.
“You’re just looking for attention.”
Accusing someone of seeking attention for their trauma symptoms reveals a fundamental misunderstanding of PTSD. This condition often drives people toward isolation and avoidance rather than attention-seeking behavior. When symptoms do become visible, it’s typically because the person is struggling significantly and may be reaching out for help. Questioning their motives can increase shame and self-doubt, potentially preventing them from accessing the support and treatment they genuinely need.
“Get over it,” or “Just snap out of it.”
Recovery from PTSD is a complex process that requires time, professional support, and often significant lifestyle adjustments. Suggesting someone should simply “get over” their trauma implies that healing is a matter of choice or willpower alone. This perspective ignores the neurobiological changes that occur with trauma and the legitimate time and effort required for recovery. Such statements can increase feelings of shame and inadequacy, potentially hindering the healing process rather than supporting it.
“People have been through worse.”
Comparing traumatic experiences dismisses the individual nature of trauma processing and recovery. The impact of a traumatic event isn’t determined solely by its objective severity but by numerous personal factors, including age, previous experiences, available support, and individual coping mechanisms. Each person’s pain deserves validation regardless of how it might compare to others’ experiences. Making comparisons can leave someone feeling guilty for struggling and questioning the validity of their own healing needs.
“Poor thing, you got triggered! You must be really sensitive!”
Being patronizing about PTSD triggers demonstrates a lack of understanding about how trauma affects the nervous system. Triggers aren’t about being “sensitive” – they’re neurobiological responses to stimuli that remind the brain of past danger. This condescending tone can feel dismissive and infantilizing, potentially damaging the person’s sense of dignity and self-worth. Understanding triggers as legitimate medical symptoms rather than character flaws is crucial for providing appropriate support.
“I know how you feel.”
While empathy is valuable, claiming to fully understand someone else’s traumatic experience can feel presumptuous and invalidating. Even individuals who have experienced similar events may process and respond to trauma very differently. Rather than assuming understanding, it’s more helpful to express genuine care and curiosity about their unique experience. This approach honors their individual journey while still offering emotional support and connection.
“Just talk it out. What’s your traumatic experience?”
Pressuring someone to discuss traumatic details before they’re ready can be retraumatizing and counterproductive. Trauma disclosure requires a sense of safety, trust, and often professional guidance to process effectively. Premature or forced discussions about traumatic events can overwhelm someone’s coping mechanisms and potentially worsen their symptoms. Respecting their pace and readiness to share demonstrates genuine care for their well-being and recovery process.
“You’re just being paranoid.”
Dismissing hypervigilance and anxiety as mere paranoia misunderstands these as legitimate trauma responses designed to protect against perceived threats. For someone with PTSD, heightened awareness and caution often feel necessary for safety, even when others don’t perceive danger. Labeling these responses as paranoid can increase self-doubt and shame, potentially preventing the person from trusting their instincts or seeking appropriate help for managing their symptoms effectively.

Best Ways to Respond to Someone With PTSD
Avoiding harmful responses is only one part of supporting someone with PTSD. Learning how to help someone with PTSD in everyday situations can guide you toward more constructive and compassionate actions.
You should encourage your friend or family member struggling with PTSD to get help from professionals in mental disorders, including PTSD. Therapists specialized in trauma-focused approaches and treatment options, such as cognitive-behavior therapy (CBT), Cognitive Processing Therapy, or Eye Movement Desensitization and Reprocessing (EMDR), can provide tailored interventions to help them process their experiences and develop coping strategies.
In the end, it’s about finding the right therapist and approach for whatever mental health or substance abuse issues the person is facing. This is especially important in cases where the connection between PTSD and depression is apparent.
Plus, connecting them with a support system or peer networks for people who have experienced similar traumas can help a person feel understood and validated. These groups can also help someone with PTSD stop feeling alienated, which goes a long way toward PTSD recovery. Women who suffer from PTSD should check out a dedicated PTSD treatment center for women.
It’s important to recognize that addressing the trauma may evoke intense emotions and reactions. Self-care practices and coping mechanisms that promote emotional regulation and relaxation — such as mindfulness exercises, deep breathing techniques, or activities that bring comfort and joy — play a vital role in combating PTSD and other mental illnesses.
Healing is a journey, and it’s okay to seek support and take breaks whenever you need to. Help foster an environment of compassion, patience, social support, and understanding. You can play a key role in aiding someone with PTSD to navigate their healing process with resilience and hope.
Addressing the Traumatic Event
When someone with PTSD opens up about their traumatic experience, the most important thing is to listen with empathy and without judgment and offer support. Your main goal must be to create a safe and supportive environment where they feel comfortable sharing their thoughts and feelings. Encourage them to talk at their own pace and reassure them that they are not alone in their struggles.
What To Do When Traumatic Events Occur
If a traumatic event occurs in the presence of someone with PTSD, it’s essential to prioritize their safety and well-being. Remain calm and reassure them, letting them know you are there to support them. Respect their boundaries and avoid pressuring them to talk about the event until they are ready. Offer practical assistance and help them access and seek professional support from the best PTSD treatment centers.
Creating a Foundation for Healing and Hope
Here’s what to do when you’re interacting with someone with PTSD:
- Listen with empathy and without judgment when someone with PTSD opens up about their experiences.
- Avoid minimizing the struggles of trauma survivors, and don’t dismiss their emotions.
- Prioritize their safety and well-being in the event of a traumatic incident, and actively prevent similar trauma where possible.
- Encourage them to seek professional help from qualified therapists specializing in trauma-focused approaches.
- Foster a supportive environment by connecting them with support groups or peer networks.
- Encourage self-care practices and coping mechanisms that promote emotional regulation and relaxation.
- Remember that healing is a journey, and seeking support and taking breaks when needed is okay.
Supporting someone with PTSD isn’t about having all the right words or perfect responses—it’s about showing up with genuine care and respect for their experience. Your presence, patience, and willingness to learn can make a profound difference in their healing journey. By choosing compassion over judgment and understanding over assumptions, you become part of their support network and contribute to creating a world where trauma survivors feel seen, valued, and empowered to heal.