Eating disorders impact millions of women, bringing severe physical and emotional challenges. This article explores the most common eating disorders affecting women, their symptoms, causes, and treatment options. Raising awareness and promoting understanding can encourage women affected by eating disorders to seek help and support.
5 Common Eating Disorders in Women
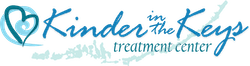
Eating disorders disproportionately affect women. In the U.S., up to 20 million women will experience an eating disorder at some point. Among young women aged 17-19, about 20.8% struggle with an eating disorder, significantly higher than their male counterparts at 5.1%.
1. Anorexia Nervosa

Symptoms: Anorexia nervosa manifests through an intense fear of gaining weight, leading to extreme food restriction, excessive weight loss, and a distorted body image. Symptoms include severe weight loss, malnutrition, brittle hair and nails, and amenorrhea (absence of menstruation).
Causes: Several factors contribute to anorexia, including societal pressures, psychological issues, and genetic predispositions. Society often glorifies thinness, creating immense pressure for women to conform to unrealistic body standards. Psychologically, individuals with anorexia may exhibit perfectionist tendencies or suffer from low self-esteem. Genetically, studies indicate that individuals with a family history of eating disorders may possess a higher risk of developing anorexia themselves.
Expert Insights: Experts emphasize the importance of early recognition and intervention. Dr. Sarah Conant, a specialist in eating disorders, notes that “early intervention significantly increases the chances of full recovery.”
Treatment Options:
- Medical Care: Addressing physical health issues like malnutrition and organ damage.
- Nutritional Counseling: Developing balanced eating habits and healthy attitudes toward food.
- Therapy: Cognitive-behavioral therapy (CBT) helps patients challenge distorted thoughts and behaviors. Family-based therapy (FBT) involves family members in the recovery process.
- Support Groups: Providing emotional support and encouragement from others who have experienced similar struggles.
2. Bulimia Nervosa

Psychological and Emotional Challenges: Bulimia nervosa involves cycles of binge eating followed by compensatory behaviors like vomiting, fasting, or excessive exercise. These cycles create significant psychological and emotional distress. Individuals with bulimia often struggle with shame, guilt, and anxiety, impacting their daily lives and mental health. The constant preoccupation with body image and weight intensifies these challenges, trapping individuals in a harmful cycle.
Cultural and Societal Influences: Cultural and societal pressures heavily influence bulimia. Media glorifies thinness, driving many to adopt unhealthy behaviors. Exposure to these pressures significantly increases the risk of bulimia, particularly among young women. The relentless pursuit of societal beauty standards makes recovery even more difficult.
Biological Factors: Genetic predispositions play a role in bulimia nervosa. Individuals with a family history of eating disorders face a higher risk. Biological factors, such as brain chemical imbalances that regulate mood and appetite, also contribute. Understanding these links helps in creating effective treatment strategies.
Expert Insights: Experts stress addressing both psychological and physiological aspects of bulimia. Dr. James Lock, a prominent researcher in eating disorders, states, “Comprehensive treatment must address the emotional and cognitive patterns driving bulimic behaviors.”
Treatment Options:
- Therapy: Cognitive-behavioral therapy (CBT) disrupts the binge-purge cycle by challenging distorted thoughts and behaviors.
- Medication: Antidepressants, especially SSRIs, reduce bulimia symptoms.
- Nutritional Counseling: Fostering healthy eating habits and attitudes toward food.
- Support Groups: Providing community and understanding among those with similar struggles.
3. Binge Eating Disorder

Cycle of Binge Eating: Binge eating disorder (BED) involves consuming large quantities of food quickly, often tied to emotional distress. Individuals feel a loss of control during binges, followed by shame and guilt. This cycle severely impacts mental and physical health, leading to obesity, heart disease, and other issues.
Genetic and Historical Aspects: Genetic factors contribute to BED. People with a family history of eating disorders have a higher risk. Historical patterns of dieting and food restriction lead to binge eating as the body reacts to deprivation with intense cravings and overeating.
Practical Tips for Management:
- Mindfulness: Practicing mindfulness helps individuals become aware of their eating habits and triggers.
- Regular Meals: Eating regular, balanced meals prevents extreme hunger that leads to binges.
- Therapy: Cognitive-behavioral therapy (CBT) helps understand and change binge eating behaviors.
- Support Networks: Connecting with support groups or therapists provides emotional support and practical advice.
Data and Research: Research shows BED affects about 3.5% of women and 2% of men in their lifetime. It is more common than anorexia and bulimia combined, highlighting the need for greater awareness and treatment options.
4. Orthorexia
Distinction Between Healthy Eating and Orthorexia: Orthorexia involves an obsessive focus on healthy eating to the point where it negatively impacts daily life. Unlike balanced healthy eating, orthorexia can lead to severe restrictions in diet and significant stress over food choices. This obsession often results in malnutrition and social isolation.
Psychological Aspects: Perfectionism drives many individuals with orthorexia. They seek control through food, believing strict diets provide a sense of order and accomplishment. This intense focus on dietary purity can lead to anxiety and guilt when deviating from their self-imposed rules.
Social and Health Consciousness Influences: Society’s increasing emphasis on health and wellness contributes to the rise of orthorexia. The proliferation of diet trends and fitness culture, often amplified by social media, pressures individuals to adopt extreme eating habits in the name of health.
Expert Insights: Dr. Steven Bratman, who first coined the term orthorexia, explains, “While the intention to eat healthily is positive, the obsession can become damaging when it begins to infringe on everyday life and well-being.”
Treatment Options:
- Therapy: Cognitive-behavioral therapy (CBT) helps address perfectionist tendencies and anxiety related to food.
- Nutritional Counseling: Restores balanced eating habits without the obsessive focus on dietary purity.
- Support Groups: Provides community and shared experiences to reduce isolation.
5. Avoidant/Restrictive Food Intake Disorder (ARFID)
Symptoms: ARFID involves eating disturbances where individuals avoid certain foods or restrict intake without concerns about body weight or shape. Symptoms include a lack of interest in eating, avoidance of foods based on sensory characteristics, and fear of negative consequences like choking.
Sensory Sensitivities and Past Experiences: Individuals with ARFID often have sensory sensitivities, making certain textures, smells, or tastes overwhelming. Past negative food experiences, such as choking or vomiting, can also contribute to the development of ARFID.
Coexisting Anxiety Disorders: Anxiety disorders frequently accompany ARFID. The fear of negative food experiences or sensory overload exacerbates anxiety, making it difficult for individuals to maintain a varied diet.
Expert Insights: Dr. Jennifer Thomas, an expert in eating disorders, states, “ARFID can severely impact a person’s ability to meet nutritional needs, leading to growth and developmental issues, especially in children.”
Treatment Options:
- Therapy: Cognitive-behavioral therapy (CBT) addresses anxiety and negative associations with food.
- Exposure Therapy: Gradual introduction of avoided foods to reduce fear and increase dietary variety.
- Nutritional Counseling: Helps develop balanced eating habits and ensures nutritional needs are met.
Seeking Help and Support
Seeking professional help for eating disorders transforms lives. Early intervention significantly boosts the chances of recovery, addressing the complex physical, psychological, and emotional aspects of these disorders. According to the National Eating Disorders Association (NEDA), early treatment can prevent severe health complications and promote long-term recovery.

Healthcare Professionals Involved:
- Therapists: Cognitive-behavioral therapy (CBT) remains the gold standard for treating eating disorders. CBT helps individuals identify and challenge harmful behaviors and thoughts, replacing them with healthier patterns. Dr. Christopher Fairburn, a leading expert in CBT for eating disorders, emphasizes its effectiveness in reducing symptoms and preventing relapse. At treatment centers like Kinder in The Keys, therapists provide CBT and other therapeutic approaches tailored to each patient’s unique needs.
- Dietitians: Specialized dietitians develop nutritional plans to restore healthy eating habits and address dietary deficiencies. They provide education on balanced nutrition and support patients in rebuilding a positive relationship with food. Kinder in The Keys includes dietitians as part of their holistic wellness practices, ensuring patients receive comprehensive nutritional care.
- Medical Doctors: Physicians play a critical role in monitoring and treating the physical health issues related to eating disorders. Regular medical evaluations ensure that patients maintain healthy body functions and receive necessary medical interventions. Treatment centers like Kinder in The Keys provide integrated medical care to address both mental and physical health.
Additional Resources:
- Hotlines: The National Eating Disorders Association (NEDA) Helpline offers immediate support and guidance for individuals and families affected by eating disorders. Accessible via phone or chat, the helpline provides confidential assistance from trained volunteers.
- Support Groups: Local and online support groups offer community and understanding. These groups, such as those facilitated by Eating Disorders Anonymous (EDA), provide a safe space for sharing experiences and gaining support from peers.
- Online Communities: Online forums and groups, such as those on the NEDA website or platforms like Reddit’s r/EatingDisorders, offer a platform for individuals to connect, share their journeys, and seek advice and encouragement.
Overcome Eating Disorders Today!
Taking the first step to seek help marks the beginning of recovery. Professional support, coupled with personal determination, paves the way for a healthier, more fulfilling life. If you or a loved one is struggling with an eating disorder, reach out to a top-rated eating disorder treatment center for support and guidance. Together, we can overcome eating disorders and embrace a brighter future.
If you found this article helpful, please share it with others who might benefit from this information. If you or someone you know is struggling with an eating disorder, seek professional help.